During the conduct of this simulation, ventricular ejection ceases completely. This form of support is not recommended in the management of most patients.
The learning objectives of the session are:
| • | To explore the cardiovascular effects of VA ECMO in a patient with cardiogenic shock. |
We will be simulating the use of a system in a patient with severe left ventricular failure – which is associated with significant respiratory impairment.
Scenario:
You are called urgently to see a 24 year-old man in the Emergency Department of your hospital. The patient had been brought in by ambulance complaining of chest pain and dyspnoea. You arrive in the department just after the patient has been intubated by the resident. The resident tells you that the patient deteriorated shortly after having a portable chest x-ray. He performed the intubation because the patient became profoundly hypotensive, unresponsive to commands and started to have frequent ventricular ectopy.
History:
According to the family, the young man had suffered a flu-like illness some weeks before and had been complaining of increasing shortness of breath and lethargy ever since. His family practitioner had prescribed two courses of broad-spectrum antibiotics and some bronchodilator therapy.
Initial Examination:
The endotracheal tube appears to be correctly positioned and breath sounds are symmetrical. The patient is hypotensive, tachycardic and has an irregular pulse. He is afebrile. His ventilation is being assisted using 100% oxygen and an Ambu © bag. Pulse oximetry indicates a saturation of ~90%.
Previous Medical History:
The family tells you that the patient has previously been in good health, that he takes no regular medications, and that he has no drug allergies. He has no relevant previous medical history.
Subsequent Management:
The patient is transferred to the Intensive Care Unit, further investigations are performed, a tentative diagnosis of viral myocarditis is made, and the decision is taken to support the patient with VA ECMO. The results of some of these investigations (Echo, ECG, CXR, and ABG) can be seen by clicking <Investigations> on the main menu.
We’ll start the tutorial by connecting the patient to our monitoring system and putting him on a ventilator.
To do this:
| • | Click the <Display> button in the <Patient Monitor> window. |
| • | Check <ECG>, <Direct Arterial Pressure>, <Central Venous Pressure> and <SaO2 and |
| • | Click the <Display> button again to close this window and display the physiological signals. |
As you can see, the patient is profoundly hypoxic (SaO2 ~ 70%) and is having frequent ventricular ectopic beats.
To ventilate the patient:
| • | Click the <Devices><Ventilator> menu item in the <Inspector> window. |
The ventilator should now appear in the <Inspector> window.
Turn the ventilator on by:
| • | Clicking the power switch at the top right-hand side of the device, and then |
| • | Setting the tidal volume (Vt) to 500 mls, the rate to 12 bpm, the FiO2 to 100% and the PEEP to 5 cms H2O. |
**Note that the ventilator’s controls are not enabled until the ventilator is turned <On>.
The ventilator is based on a simple anaesthesia system which is in ‘Synchronised Intermittent Mandatory Ventilation’ (SIMV) mode.
In order to assess the patient’s gas exchange you may want to:
Turn on the gas analyser:
| • | Click the <Display> button in the <Patient Monitor> window. |
| • | Check < Capnography > and < Gases > in the <Display> window. |
| • | Click the <Display> button again to close this window and display the additional signals. |
And perform a baseline blood gas analysis:
| • | Click <Investigations><Arterial Blood Gas Analysis>in the <Inspector> window. |
You may also wish to paralyse the patient and control his ventilation. To do this:
| • | Click <Bolus Drug><Pancuronium (2mg/ml)>in the <Therapeutic Interface> window. |
| • | Drag the green slider until it says ~ 8 mgs and click the <Give> button. |
If you wish to monitor the onset of muscle paralysis by monitoring his ‘Train of Four’:
| • | Click the <Devices><Nerve Stimulator> menu item in the <Inspector> window. |
| • | Click the <TOF> button on the nerve stimulator itself. |
Sedation may be administered by selecting the appropriate bolus or infusion drugs using the <Therapeutic Interface> and monitoring the depth of sedation by turning on the <BIS> display on the physiological monitor.
An inotrope can also be administered using the <Therapeutic Interface>.
You elect to cannulate the patient percutaneously via the right femoral artery and vein using the Seldinger technique and ultrasonic guidance.
Imagine now that you have:
| • | Placed the Seldinger wires in the artery and vein, |
| • | Given the patient 7500 units of heparin (<Therapeutic Interface> <Bolus Drug> <Heparin> <Give> 7500 units) and |
| • | Positioned the cannulae under ultrasonic control. |
The cannulae have been connected to the ECMO system. The entire system is heparin-coated. The system’s centrifugal pump is responsible both for generating the negative pressure which is required to facilitate drainage and the positive pressure which is required to pump blood through the artificial lung and back into the patient. The pump head and oxygenator are integrated into a single, disposable unit which is mounted on the system console (Figure 1.).
Figure 1.
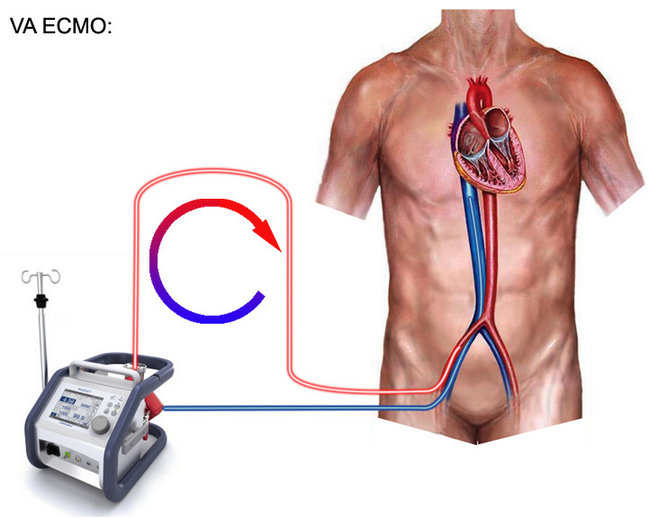
Active venous drainage from the right atrium is via the 24F venous cannula and return via the 21F arterial cannula. A femoral ‘backflow’ cannula has not been used. Additional information regarding the ECMO system can be found by clicking on the <Resources> menu of the <Inspector> window and selecting the resource which you want to view. These resources include lectures on ECMO, images of various systems, relevant websites and various descriptions and protocols relating to the technique.
To visualize the ECMO interface itself:
| • | Click on <Devices><ECMO System> menu item of the <Inspector> window. |
The key features of the ECMO system have been outlined in the tutorials entitled “VA ECMO Tutorial 1” and “VV ECMO Tutorial 1”. Refer to these examples for an explanation of the use of the system.
Before commencing VA ECMO you may wish to confirm that the patient is effectively anti-coagulated ( <Devices><ACT Monitor> <Start>). If you do this, you’ll need to click <Devices><ECMO System> to return to the ECMO interface. (You can periodically return to the ACT Monitor to check on the progress of the estimation). Give more Heparin if you think it is needed.
We’re now nearly ready to commence VA ECMO. To complete our preparations we need to:
| • | Click <Devices><ECMO System> and select the <VA ECMO> option at the bottom right of the interface. |
| • | Click the <Adjust Cannula> button and advance the drainage cannula as far as it will go using the slide control on the left hand side of the window. |
| • | Re-open the ECMO interface by clicking <Devices><ECMO System>. |
| • | Click the <Main Power> button at the top right of the interface. |
| • | Turn on 6 LPM of oxygen using the middle knob at the left of the interface. |
At this point we’re ready to initiate ECMO. However, we must remember that, unlike the case for VV ECMO, there is a pressure gradient across the circuit and if we simply open the clamp, blood will flow from the arterial side of the circuit to the venous side and a large left-to-right shunt will be created.
In order to avoid this effect, we need to generate a stagnation pressure that is a little bit above the patient’s mean arterial pressure. To do this:
| • | Slowly turn up the flow control until the indicated pressure is ~ 10 mm Hg above the patient’s mean arterial pressure with the clamp still fully closed. |
| • | Progressively release the arterial clamp by moving the slide control upwards. |
Observe that flow increases to about 1 lpm. Now:
| • | Increase the flow further by slowly rotating the flow control. |
Note how the patient’s pulse pressure becomes progressively smaller until it eventually disappears altogether (at a flow of about 4.0 lpm). What’s happening here? - Well, as we steadily increase ECMO flow, so we progressively deprive the left ventricle of more and more of its inflow (preload), until the point is reached where it has none at all, and ejection ceases. At this point the patient is on full cardio-pulmonary bypass (CPB), there is no flow through the pulmonary circulation or the left side of the heart and the aortic valve remains closed throughout the cardiac cycle.
The ‘Rule of Thumb’ which describes the relationship between ECMO flow rate and LV preload can be summarized as:
LV Preload is proportional to 1/ECMO Flow.
Or, in plain language: “Left ventricular preload decreases with increasing ECMO flow rate.” This ‘Rule of Thumb’ can be contrasted with the relationship between ECMO flow rate and LV afterload, where:
LV Afterload is proportional to ECMO Flow.
Or, in plain language: “Left ventricular afterload increases with increasing ECMO flow. ”
The situation of the patient on full VA ECMO differs from the patient on full (surgical) bypass in two important respect s:
| • | The circuit does not include a venous drainage reservoir and, |
| • | Venous drainage is ‘active’ rather than ‘passive’. |
The presence of a venous reservoir in a surgical CPB circuit allows the perfusionist to control LV preload relatively independently of main pump flow (by adjusting the volume of blood in the reservoir). In contrast, during VA ECMO, the perfusionist can only adjust LV preload by changing the main pump flow rate. As a result, ‘tight’ control of systemic blood pressure is more difficult to achieve during VA ECMO than during surgical CPB.
In this simulation, note how the mean arterial pressure (MAP) has risen from ~ 65 mm Hg before bypass to ~ 105 mm Hg. This higher mean pressure reflects the fact that the patient’s total systemic flow (LV output + ECMO output) is now higher than before ECMO and that the patient’s Systemic Vascular Resistance (SVR) is little changed. As a result, mean arterial pressure is considerably higher.
Under normal circumstances, if we were on surgical CPB, we would respond to this scenario by temporarily reducing the arterial pump flow at the same time as minimizing left ventricular (LV) preload by ensuring that drainage into the venous reservoir was unimpeded. However, during VA ECMO, if we reduce blood flow rate, we will divert more flow through the pulmonary circulation, increase LV preload, and the left ventricle will begin to eject again. In practice, we can only adjust SVR by the use of vaso-dilator or constrictor therapy and we can only adjust circulating blood volume by fluid administration or diuretic therapy.
After a few minutes, perform a blood gas analysis:
| • | <Investigations><Arterial Blood Gas Analysis> |
And note that the PaO2 is now ~ 500 mm Hg and that the PaCO2 is within the normal range. These results are typical for a normally-functioning VA ECMO system when 100% oxygen is administered under full bypass conditions. It is debatable whether or not a patient should be maintained on full bypass if clinically satisfactory conditions can be obtained by using only partial support.
Full bypass abolishes pulmonary arterial flow and entails the risks of left heart distension, pulmonary or left heart thrombosis and coronary ischaemia (due to increased left ventricular wall stress).
In contrast, partial bypass maintains pulmonary flow and reduces the risks of left heart distension and thrombosis, but creates the possibility of differential hypoxia and the requirement for some form of ongoing ventilation.
Finally, we’ll examine the effect of the administration of a powerful vasodilator (Sodium Nitroprusside (SNP)) on the behaviour of the EMO system.
Commence an infusion of SNP by:
| • | Selecting <Therapeutic Interface> <Infusion Drug> <SNP (100mcg/ml)> |
And starting it at 20 ml/hr:
| • | Slide green slider to <20> and click <Set> |
After about 5 minutes, note that the:
| • | Mean arterial pressure has fallen to 65 – 70 mm Hg; |
| • | The pump flow rate has increased to ~ 5 lpm and |
| • | The CVP has fallen. |
Why is this so? The SNP is both an arterial and veno-dilator. As the plasma level of the drug rises, so SVR and MAP both fall. As a result, it is now ‘easier’ for the ECMO system to pump and so pump output increases despite the fact that the rpm remain unchanged. The CVP also falls because of the veno-dilatation induced by the drug.
This concludes VA ECMO tutorial 2.