Some of the manoeuvres performed in this simulation must never be performed on a real patient.
The learning objectives of the session are:
| • | To recognise the signs of oxygenator failure. |
We will be simulating the use of a system in a patient with severe left ventricular failure – which is associated with significant respiratory impairment.
Scenario:
You are called urgently to see a 24 year-old man in the Emergency Department of your hospital. The patient had been brought in by ambulance complaining of chest pain and dyspnoea. You arrive in the department just after the patient has been intubated by the resident. The resident tells you that the patient deteriorated shortly after having a portable chest x-ray. He performed the intubation because the patient became profoundly hypotensive, unresponsive to commands and started to have frequent ventricular ectopy.
History:
According to the family, the young man had suffered a flu-like illness some weeks before and had been complaining of increasing shortness of breath and lethargy ever since. His family practitioner had prescribed two courses of broad-spectrum antibiotics and some bronchodilator therapy.
Initial Examination:
The endotracheal tube appears to be correctly positioned and breath sounds are symmetrical. The patient is hypotensive, tachycardic and has an irregular pulse. He is afebrile. His ventilation is being assisted using 100% oxygen and an Ambu © bag. Pulse oximetry indicates a saturation of ~80%.
Previous Medical History:
The family tells you that the patient has previously been in good health, that he takes no regular medications, and that he has no drug allergies. He has no relevant previous medical history.
Subsequent Management:
The patient is transferred to the Intensive Care Unit, further investigations are performed, a tentative diagnosis of viral myocarditis is made, and the decision is taken to support the patient with VA ECMO. The results of some of these investigations (Echo, ECG, CXR, and ABG) can be seen by clicking <Investigations> on the main menu.
We’ll assume that you have already worked your way through the previous VA ECMO tutorials, so quite quickly we’ll:
Set up our monitoring:
| • | Click the <Display> button in the <Patient Monitor> window. |
| • | Check <ECG>, <Direct Arterial Pressure>, <Central Venous Pressure> and <SaO2> and |
| • | Click the <Display> button again to close this window and display the physiological signals. |
Ventilate the patient:
| • | Click the <Devices><Ventilator> menu item in the <Inspector> window. |
| • | Click the power switch at the top right-hand side of the device, and then set the tidal volume (Vt) to 500 mls, the rate to 12 bpm, the FiO2 to 100% and the PEEP to 5 cms H2O. |
Paralyse the patient:
| • | Click <Bolus Drug><Pancuronium (2mg/ml)>in the <Therapeutic Interface> window. |
| • | Drag the green slider until it says ~ 8 mgs and click the <Give> button. |
And perform a baseline blood gas analysis:
| • | Click <Investigations><Arterial Blood Gas Analysis>in the <Inspector> window. |
You elect to cannulate the patient percutaneously via the right femoral artery and vein using the Seldinger technique and ultrasonic guidance.
Imagine now that you have:
| • | Placed the Seldinger wires in the artery and vein, |
| • | Given the patient 7500 units of heparin (<Therapeutic Interface> <Bolus Drug> <Heparin> <Give> 7500 units) and |
| • | Positioned the cannulae under ultrasonic control. |
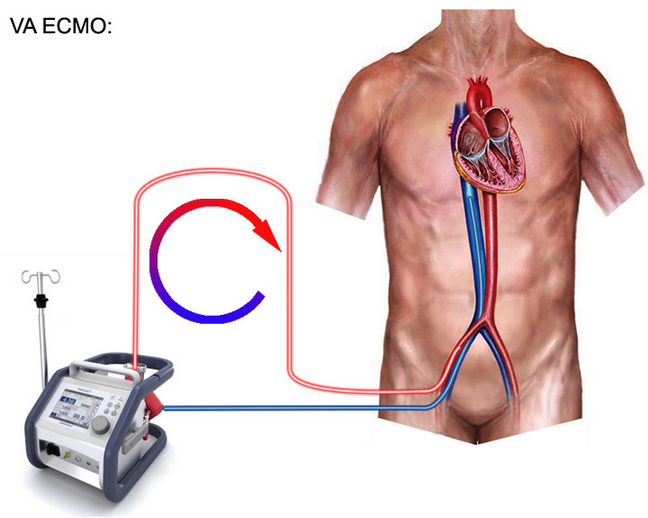
The cannulae have been connected to the ECMO system. The entire system is heparin-coated. The system’s centrifugal pump is responsible both for generating the negative pressure which is required to facilitate drainage and the positive pressure which is required to pump blood through the artificial lung and back into the patient. The pump head and oxygenator are integrated into a single, disposable unit which is mounted on the system console (Figure 1.).
Figure 1.
We’re now nearly ready to commence VA ECMO. To complete our preparations we need to:
| • | Click <Devices><ECMO System> and select the <VA ECMO> option at the bottom right of the interface. |
| • | Click the <Adjust Cannula> button and advance the drainage cannula as far as it will go using the slide control on the left hand side of the window. |
| • | Re-open the ECMO interface by clicking <Devices><ECMO System>. |
| • | Click the <Main Power> button at the top right of the interface. |
| • | Turn on 6 LPM of oxygen using the middle knob at the left of the interface. |
To initiate VA ECMO:
| • | Turn up the <RPM> until the stagnation pressure is ~ 10 mm Hg > the patient’s mean arterial pressure. |
| • | Fully open the <arterial clamp> by sliding the slider upwards. |
| • | Now slowly further increase the <RPM> until a flow rate of 5 lpm is achieved. |
| • | Start the <Timer> (on the physiological monitor). |
The mean arterial pressure is very high, but for the purposes of this exercise, we’ll just accept it.
After five minutes:
| • | Perform an <Arterial Blood Gas Analysis>, |
| • | Perform an <Oxygenator Blood Gas Analysis> and |
| • | Return to the <ECMO System>. |
As there is no ventricular ejection, there is little difference between the arterial and oxygenator samples. In both cases, the PO2 should be about 400 mm Hg and the PCO2 about 35 mm Hg. Note, also that the pre-membrane pressure is ~ 305 mm Hg and that the rpm are about 3500.
Now, ask the Supervisor to cause the oxygenator to fail **.
Over the next few minutes, observe that:
| • | The pre-membrane pressure has risen to ~ 330 mm Hg, |
| • | The blood flow has fallen to ~ 3.5 lpm and that |
| • | Some ventricular ejection has become apparent. |
Start the <Timer> and after five minutes::
| • | Repeat the <Arterial Blood Gas Analysis> and |
| • | Repeat the <Oxygenator Blood Gas Analysis>. |
Note that the Arterial and Oxygenator PO2 has fallen precipitously to about 45 mm Hg and that the PCO2 has risen by about 10 mm Hg to ~ 47.
How can we interpret these results?
We suspect that the oxygenator is becoming partially occluded by the deposition of fibrin and/or thrombus. As a result, the pre-membrane pressure is rising and the delivered flow falling. (If we were to measure the pressure drop across the oxygenator, we would see that it had increased.) The gas transfer function of the oxygenator is also failing. (The supervisor has ‘failed’ about 50% of the membrane). As a result, the PO2 is falling and the PCO2 rising.
These results are typical of one of the more common forms of oxygenator failure and can be summarized as:
| • | Elevation of the pre-membrane pressure, |
| • | Reduction of the blood flow rate - in association with |
| • | Hypoxia and |
| • | Hypercarbia. |
In real life, how can we think about oxygenator failure?
One method is to classify it according to the mechanism of failure of the oxygenator. Using this approach, we can identify three categories:
| • | Failure of gas transfer function, |
| • | Failure of structural integrity and |
| • | Failure of heat transfer function. |
In the example given above, the oxygenator failure is manifest as both a failure of gas transfer function and as a failure of structural integrity (the membrane resistance has increased).
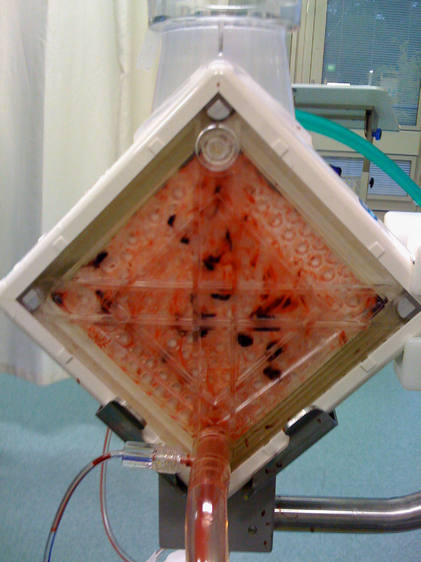
Fibrin or thrombus deposition is one of the most common causes of this type of oxygenator failure in ECMO systems which use non-porous, polymethylpentene, hollow-fibre membrane systems (Figure 2.).
Figure 2.
In contrast, the older, micro-porous, polypropylene, hollow-fibre systems were prone to plasma leakage which occurred much earlier in the life-cycle of the device. An example of this is shown in figure 2.
Figure 2.
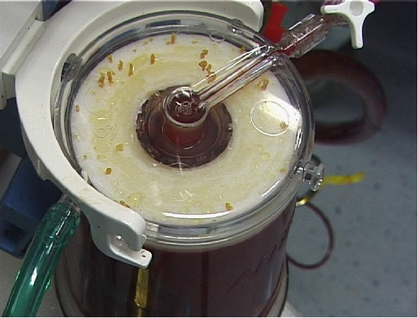
In this case, plasma leakage was associated with a significant degree of gas transfer failure which necessitated an urgent oxygenator change out.
This concludes VA ECMO Tutorial 4.
** Supervisor’s note:
| • | Increase Oxygenator <Qs/Qt> to 0.5, |
| • | <Vd/Vt> to 0.5 and |
| • | <Membrane Resistance> to 50 mm Hg/L/Min |
over the course of a few minutes.